* **Sleep paralysis**
* Transitions between REM sleep and wakefulness
Nocturnal immobility happens when this mechanism fails to disengage on time.
In simple terms:
> The brain wakes up before the body gets the message.
—
## Why the Body “Refuses” to Move
The sensation feels like betrayal—like the body has suddenly turned against you. But in reality, it’s doing exactly what it evolved to do.
### REM Atonia: The Brain’s Safety Lock
During dreaming, the brain activates vivid imagery, emotions, and narratives. To keep us safe, it simultaneously activates **REM atonia**, a state in which most voluntary muscles are inhibited.
The result is a strange limbo:
* Conscious mind
* Immobile body
* Heightened fear response
The mismatch is deeply unsettling because the human nervous system is not designed to experience wakefulness without movement.
—
## The Role of Fear and the Amygdala
One reason nocturnal immobility feels so terrifying is neurological.
When the brain wakes suddenly in paralysis:
This is why many people report:
* A sense of danger or presence
* Intense dread
* The feeling of being watched
The fear is not imagined—it is *neurologically amplified*.
Your brain is in survival mode without context.
—
## Hallucinations: When Dreams Bleed Into Reality
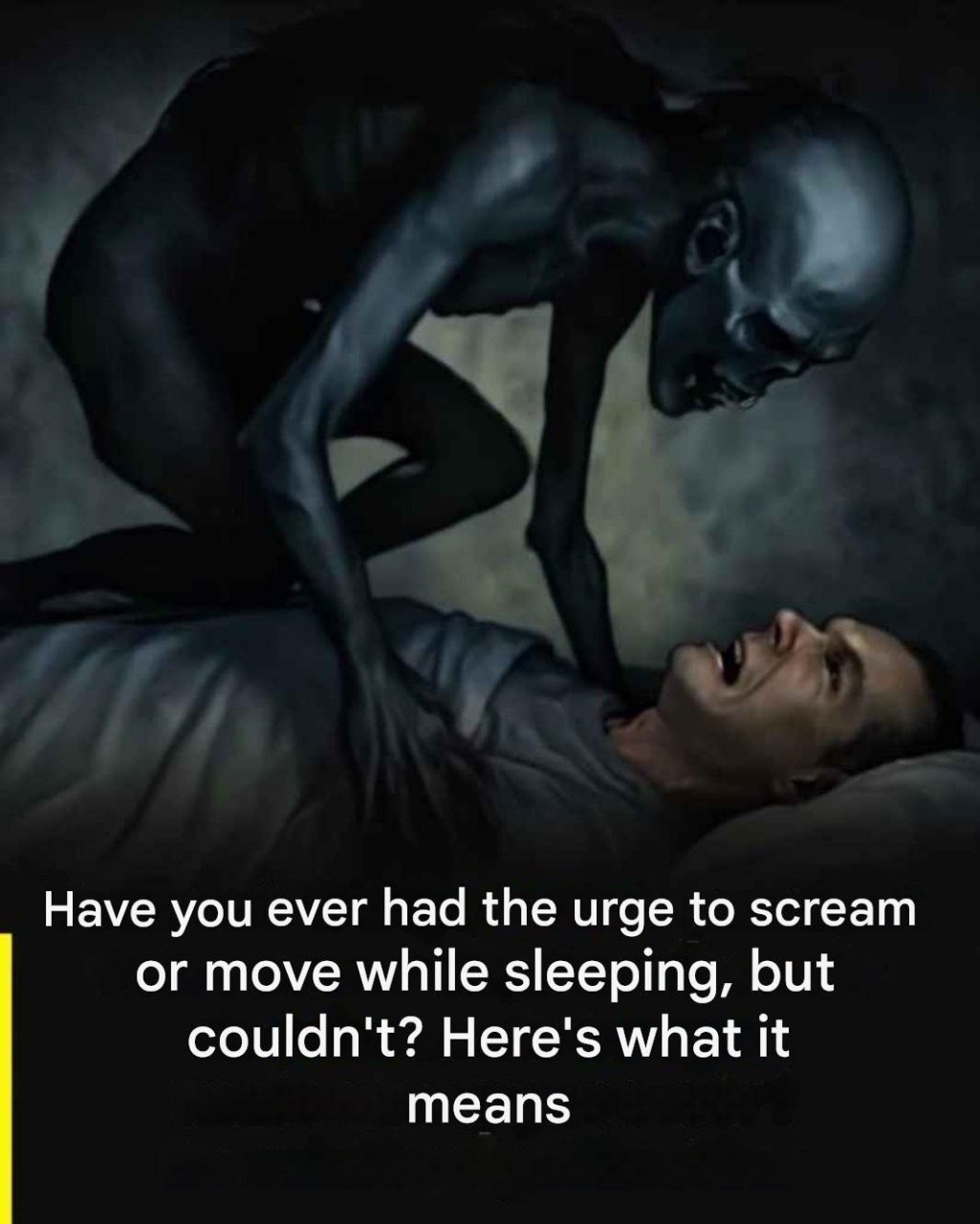
One of the most haunting aspects of nocturnal immobility is the hallucinations.
People commonly report:
* Shadowy figures
* Pressure on the chest
* Whispering or footsteps
* A presence in the room
* The feeling of being touched
These experiences are known as **hypnagogic or hypnopompic hallucinations**, depending on whether they occur while falling asleep or waking up.
They happen because:
* The dream imagery system is still active
* Sensory input is partially suppressed
* The mind attempts to explain paralysis using narrative
The brain fills the gap.
And it often fills it with fear.
—
## Why the Experience Feels So Personal
Nocturnal immobility doesn’t feel like a neutral medical event.
It feels **targeted**.
That’s because the hallucinations often align with personal fears, cultural beliefs, and emotional states. A medieval European might have seen a witch. Someone today might see an intruder, an alien, or a shadow figure.
The brain uses familiar symbols to make sense of confusion.
The experience feels meaningful because the mind is wired to seek meaning—even in error.
—
## Who Is Most Likely to Experience It?
Sleep paralysis is surprisingly common. Studies suggest that **up to 40% of people experience it at least once** in their lifetime.
It is more likely to occur in individuals who:
* Have irregular sleep schedules
* Experience chronic stress or anxiety
* Have disrupted circadian rhythms
* Sleep on their back
* Experience sleep deprivation
* Have a family history of sleep disorders
It often first appears during adolescence or early adulthood, when sleep patterns are in flux.
—
## The Emotional Aftermath
Even when people know what happened, the emotional impact can linger.
Common reactions include:
* Fear of falling asleep again
* Hypervigilance at night
* Anxiety about “losing control”
* Questioning reality or sanity
The episode may last seconds or minutes—but the memory can last years.
This is because the experience bypasses rational processing and imprints directly into emotional memory.
—
## Why Knowledge Alone Isn’t Always Comforting
Many people are told, “It’s just sleep paralysis. It’s harmless.”
While that is medically true, it often misses the emotional reality.
Knowing what happened doesn’t automatically neutralize:
* The terror
* The vulnerability
* The sense of helplessness
Because nocturnal immobility attacks something fundamental: **agency**.
The inability to move, speak, or escape triggers primal fear—regardless of explanation.
—
## Learning to Reclaim Control
While there is no single cure, there are ways to reduce both frequency and fear.
### Improving Sleep Stability
* Maintain a consistent sleep schedule
* Avoid sleep deprivation
* Reduce caffeine and alcohol before bed
### Changing Sleep Position
Many people experience fewer episodes when avoiding sleeping on their back.
### Managing Stress
High emotional stress increases REM fragmentation, making overlap states more likely.
Mindfulness, therapy, or stress-reduction practices can help stabilize sleep architecture.
—
## What to Do During an Episode
If you find yourself trapped in nocturnal immobility, there are strategies that may help shorten the experience:
* Focus on slow breathing
* Try to move a small muscle (tongue or toes)
* Remind yourself it will pass
* Avoid fighting violently—it increases panic
The paralysis always ends.
The body always reawakens.
—
## When to Seek Professional Help
Occasional episodes are usually benign. But medical advice is recommended if:
* Episodes are frequent or worsening
* Daytime sleepiness is severe
* There are symptoms of narcolepsy
* Fear begins to interfere with sleep regularly
Sleep disorders are treatable—and support matters.
—
## The Deeper Meaning We Attach to It
Throughout history, nocturnal immobility has been interpreted as:
* Spiritual attack
* Psychological weakness
* Supernatural encounter
Today, science reframes it as a neurological boundary glitch.
But the experience still raises profound questions:
* What is consciousness?
* Where does the self reside?
* How fragile is our sense of control?
For a moment, the illusion of mastery over the body dissolves.
And that can be deeply unsettling.
—
## Final Thought: Between Waking and Dreaming
The enigma of nocturnal immobility exists in a narrow space—between sleep and waking, control and surrender, biology and fear.
It reminds us that consciousness is not a switch, but a spectrum. That the body and mind do not always rise together. And that even in moments of paralysis, the experience itself is temporary.
The body is not refusing to obey.
It is simply caught between worlds—doing its best to protect you, even when it doesn’t feel that way.
And when movement finally returns, what lingers most is not fear—but awe at how thin the line truly is between dreaming and being awake.
—
If you’d like, I can:
* Add scientific references and studies
* Rewrite this in a more poetic or more clinical tone
* Adapt it for a psychology, neuroscience, or wellness blog
* Shorten it into a viral or story-based version