The phrase “denying care” can be misleading. In many cases, it’s not a clear-cut refusal but a complicated interaction between fear, autonomy, and systemic barriers.
### Fear of Medical Systems
### Financial Anxiety
Even with insurance or government assistance, many seniors fear medical bills. The anxiety around cost can lead people to delay or avoid care altogether.
### Cognitive Decline
Conditions like dementia, delirium, or untreated mental illness can impair judgment. What appears to be a refusal may actually be confusion or inability to understand the consequences.
### Desire for Control
For some, refusing care is a way to assert autonomy in a world where independence is slipping away. Saying “no” can feel like the last remaining form of control.
—
## When Autonomy and Protection Collide
Adults—even elderly ones—have the legal right to refuse medical treatment, provided they are deemed mentally competent. But determining competence in crisis situations is not always straightforward.
First responders, social workers, and healthcare professionals often face impossible choices:
* Respect a person’s stated wishes
* Or intervene against those wishes to prevent harm
When systems are underfunded and overstretched, these decisions become even harder.
—
## The Role of Social Isolation
Social isolation is a silent but deadly factor in many elderly deaths.
* Notice declining health
* Advocate for medical care
* Ensure medications are taken properly
* Recognize confusion or distress
Isolation can turn manageable health issues into fatal ones.
In motel settings, isolation is often compounded by transience. Neighbors come and go. Staff may not be trained to recognize medical emergencies beyond the obvious. Warning signs can be missed until it’s too late.
—
## A Broader Systemic Failure
While individual choices matter, stories like this also point to systemic issues that extend far beyond one person or one incident.
### Gaps in Elder Care Services
Many communities lack adequate outreach programs for seniors living independently but precariously. Home visits, wellness checks, and case management services are often limited or difficult to access.
### Housing Insecurity Among Seniors
Rising housing costs disproportionately affect elderly people on fixed incomes. When rent becomes unaffordable, motels and temporary housing become last resorts.
### Overburdened Healthcare Systems
Emergency rooms and clinics are often ill-equipped to provide the time and attention complex elder cases require. This can leave seniors feeling rushed, unheard, or reluctant to return.
—
## The Human Cost Behind the Statistics
It’s easy to talk about policy, systems, and trends. Harder—but more important—is remembering that each story represents a human life.
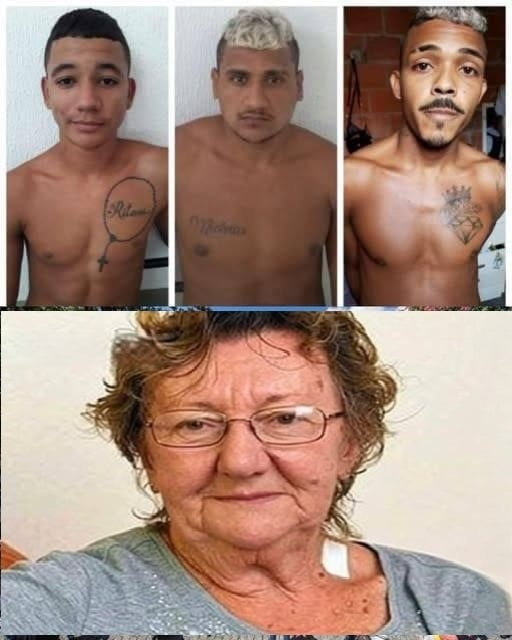
An elderly woman who died alone in a motel was not just a headline. She was someone who had lived decades of experiences:
* She may have raised children
* Loved deeply
* Worked hard
* Survived losses and challenges
Her death, regardless of circumstances, deserves dignity and reflection.
—
## Media Responsibility and Public Reaction
Sensational or incomplete headlines can unintentionally shift focus away from compassion and toward judgment.
Public reactions often fall into two camps:
* Blaming the individual for refusing care
* Blaming institutions or responders for not doing more
Reality usually lies somewhere in between.
Responsible reporting should encourage empathy and inquiry—not outrage without understanding.
—
## What Can Be Learned From Tragedies Like This?
While no lesson can undo a loss, stories like this can push us to ask better questions and demand better solutions.
### For Communities
* Are there seniors living invisibly in temporary housing?
* Are wellness checks and outreach programs adequately funded?
* Do local businesses and staff know how to recognize distress in elderly individuals?
### For Families
* Are we checking in on older relatives consistently?
* Do they understand their medical options and rights?
* Do they have someone advocating for them if they can’t advocate for themselves?
### For Policymakers
* Is elder care being prioritized in housing and healthcare policy?
* Are mental health and cognitive assessments accessible to seniors?
* Are end-of-life care discussions normalized and supported?
—
## The Importance of Early Intervention
Many tragedies are not the result of a single decision, but of long chains of neglect, delay, and missed opportunities.
Early intervention—medical, social, and emotional—can prevent situations from reaching crisis points. That requires investment, coordination, and a cultural shift in how we view aging.
—
## Aging With Dignity Should Not Be a Privilege
Perhaps the most painful truth highlighted by stories like this is that aging with dignity is not guaranteed—it’s often dependent on income, family support, and geography.
A society is often judged by how it treats its most vulnerable. Elderly individuals who die alone, in temporary housing, after denying or lacking care, reveal uncomfortable truths about where support systems fail.
—
## Final Thoughts
The headline *“Elderly woman dies in motel after denying care”* is more than a tragic news item—it’s a mirror reflecting larger societal challenges.
It asks us to consider:
* How we support aging individuals
* How we balance autonomy with protection
* How easily people can become invisible
Above all, it reminds us that compassion must extend beyond blame. Understanding, prevention, and meaningful support are the only ways to ensure that fewer lives end this way.
Every elderly person deserves safety, dignity, and care—regardless of where they live or the choices they make in moments of fear or uncertainty.
If you’d like, I can also write:
* A **policy-focused analysis on elder care failures**
* A **human-centered narrative essay**
* Or a **guide on recognizing warning signs in isolated seniors**
Just tell me how you’d like to continue the conversation.